Vitamin D Deficiency Doubles Risk of Developing Schizophrenia
A new meta-analysis of observational studies focused on the possible relationship between vitamin D serum levels and the odds of developing schizophrenia has concluded that a strong association exists between vitamin D deficiency and schizophrenia.
The research was conducted and authored by Doctors Ghazaleh Valipour, Parvane Saneei, and Ahmad Esmaillzadeh of the Food Security Research Center and Department of Community Nutrition, School of Nutrition and Food
Science, Isfahan University of Medical Sciences in Isfahan, Iran, respectively. The analysis involved a comprehensive review of 19 previous studies involving in excess of 2,800 total participants. The original article outlining the research debuted recently in the Journal of Clinical Endocrinology and Metabolism.

The researchers defined schizophrenia as a group set of neuropsychiatric disorders characterized by symptoms like hallucinations, delusions, confused thinking and disorganized speech.
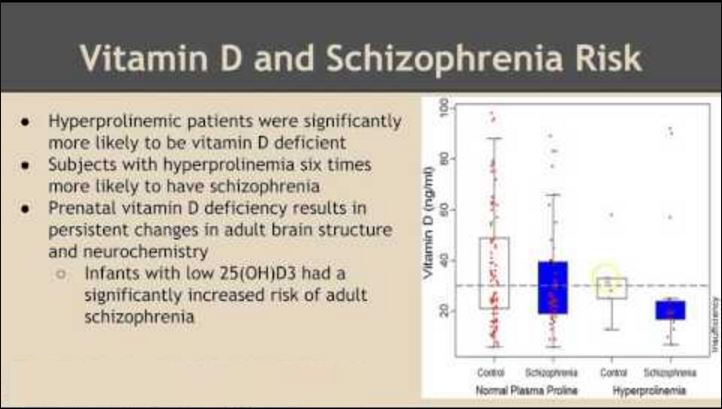
Upon careful review of 19 previously conducted studies from around the world, the researchers concluded that individuals who suffer from vitamin D deficiency (vitamin D serum levels deemed lower than is considered healthy by accepted medical science) are more than twice as likely to develop schizophrenia than their vitamin D sufficient (healthy levels of vitamin D serum) counterparts. Specifically, the scientists found that inadequate levels of vitamin D increased the risk of developing schizophrenia by 2.16 times that associated with an individual whose vitamin D levels are within a healthy range.
Of those who had already been diagnosed with the mentally debilitating psychiatric condition, 65% were found to have insufficient levels of vitamin D.
The researchers stopped short of declaring that vitamin D supplementation may help to reduce the risk of developing the condition. Rather, they cautioned that more research would be necessary to observe the effects of supplementation on schizophrenia and its manifestation in previously healthy individuals. They also stopped short of declaring supplementation a means of treating existing schizophrenia, again alluding to the need for further study.
The abstract of the study can be viewed here: http://press.endocrine.org/doi/pdf/10.1210/jc.2014-1887.
 A 1991 study² showed “significant improvement” in 68 of 83 patients exhibited of their psoriatic lesions with the topical application of vitamin D3.” 24 of 35 patients treated with oral vitamin D3 showed improvements, according to the same study.
A 1991 study² showed “significant improvement” in 68 of 83 patients exhibited of their psoriatic lesions with the topical application of vitamin D3.” 24 of 35 patients treated with oral vitamin D3 showed improvements, according to the same study.
 In the editorial opinion of the Vitamin D3 Blog, sufficient evidence exists to justify the use of both topical and oral vitamin D3 supplements for the treatment of mild-to-moderate plaque psoriasis. These are available in multiple forms, but it is the opinion of this blog that with regard to D3 supplements, it is worth spending a couple of extra dollars to ensure top quality as vitamin D is one of the nutrients for which the effectiveness can vary relative to the quality of the manufacturing process and supplement ingredients.
In the editorial opinion of the Vitamin D3 Blog, sufficient evidence exists to justify the use of both topical and oral vitamin D3 supplements for the treatment of mild-to-moderate plaque psoriasis. These are available in multiple forms, but it is the opinion of this blog that with regard to D3 supplements, it is worth spending a couple of extra dollars to ensure top quality as vitamin D is one of the nutrients for which the effectiveness can vary relative to the quality of the manufacturing process and supplement ingredients.
 Unlike a traditional study, the research published July 22 in the Journal of Clinical Endocrinology and Metabolism constitutes what is known as a “meta analysis”. In a meta analysis, unlike a traditional experiment, study or clinical trial, instead of conducting original research using volunteers (test subjects), a control group and different variables to determine how the different variables react (or don’t react) to the volunteers under various circumstances; the researchers instead review previously conducted research. The objective is to review numerous studies which are similar in nature in an attempt to discern any patterns or other data that may surface in the presence of macro-data that may not be as obvious within the context of a single study.
Unlike a traditional study, the research published July 22 in the Journal of Clinical Endocrinology and Metabolism constitutes what is known as a “meta analysis”. In a meta analysis, unlike a traditional experiment, study or clinical trial, instead of conducting original research using volunteers (test subjects), a control group and different variables to determine how the different variables react (or don’t react) to the volunteers under various circumstances; the researchers instead review previously conducted research. The objective is to review numerous studies which are similar in nature in an attempt to discern any patterns or other data that may surface in the presence of macro-data that may not be as obvious within the context of a single study. Every time you microwave a lean cusisine or TV dinner, the heat from the microwave radiates the plastic, releasing BPA (Bisphenol A, an ingredient found in Polycarbonate plastics as well as epoxy resins) and dioxins, both of which disrupt hormone function.
Every time you microwave a lean cusisine or TV dinner, the heat from the microwave radiates the plastic, releasing BPA (Bisphenol A, an ingredient found in Polycarbonate plastics as well as epoxy resins) and dioxins, both of which disrupt hormone function.
 tamin D3
tamin D3

